Coeliac Disease
What is Coeliac disease?
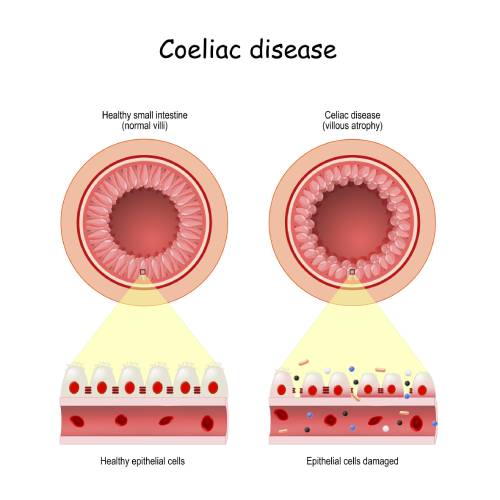
Coeliac disease is an autoimmune condition in which the body reacts abnormally to a food protein called ‘gluten’. The body’s immune system wrongly identifies gluten as potentially dangerous and mounts an immune response which causes inflammation and damage to the lining of the small bowel.
Approximately 1% of the Australian population is affected with coeliac disease.
What causes Coeliac disease?
The genes responsible for coeliac disease are located on chromosome 6 which codes for two genes intimately involved in coeliac disease: HLA-DQ2 and HLA-DQ8. 95% of people with coeliac disease are positive for either HLA-DQ2 or HLA-DQ8 (1). These genes are most often found in people of Northern European descent (Ireland, Scotland, Scandinavia, Germany), however these genes have been found in people of all ethnicities (2).
In addition to genetics, environmental factors such as diet and exposure to certain infections are thought to play a role. A Swedish study, for example, demonstrated that if an infant is introduced to higher amounts of gluten in the first 12 months of life, they were more likely to develop coeliac disease (3).
Unfortunately, the incidence of coeliac disease appears to be increasing worldwide (2).
What are the symptoms and complications of Coeliac disease?
The classic symptoms of coeliac disease include:
– abdominal pain
– bloating
– diarrhoea
Only about 50% of people with Coeliac disease have these classic symptoms and indeed some patients have no symptoms at all. Additional but less common symptoms include:
– nausea / vomiting
– weight loss
– constipation
– belching / flatulence
– fatigue / weakness
– headaches and difficulty concentrating: ‘ brain fog ‘
A classic skin rash called dermatitis herpetiformis is seen in about 10% of coeliac patients. It is usually under the elbows and is very itchy. Joint pain and muscle cramps can also occur.
Complications of coeliac disease include:
– vitamin and mineral deficiencies – these include iron, calcium, vitamin B12, folate, vitamin D and zinc
– osteoporosis (linked to calcium deficiency)
– weight loss
– lymphoma of the small bowel
– infertility in both men and women (4)
– poor growth in children and delayed puberty in teenagers (5)
How do you diagnose Coeliac disease?
The diagnosis of coeliac disease requires 2 things:
1- A positive blood test for coeliac antibodies
2- A biopsy of the small bowel showing coeliac type damage to the small bowel
For both of these tests to be accurate, you need to be on a gluten-containing diet at the time of testing. Otherwise, there is a risk of a false negative result.
The most common and reliable blood antibody test is tissue Transglutaminase (tTG) (6). In special circumstances your doctor may order other blood tests which include ENA, Anti-gliadin, Anti-DAP, and HLA-DQ2/HLA-DQ8 testing.
The small bowel biopsy is obtained through a gastroscopy. This procedure is done by a Gastroenterologist which involves passing a tiny flexible camera through the mouth and down into the first part of the small bowel (duodenum). Tissue samples are taken with biopsy forceps (2mm tissue samples). The procedure takes 5 mins and you are given sedation to make you comfortable.
There is also a second blood test called a ‘gene’ test that identifies if you carry one of the susceptible genes (HLA-DQ2/DQ8). This test does not require a diet containing gluten to be consumed, and it is most helpful in ruling out coeliac disease especially if gluten has already been eliminated from the diet. A positive gene test only indicates that you carry the gene(s) and have a susceptibility for coeliac disease.
Coeliac disease is associated with other conditions and if you have coeliac disease you should be screened for:
–Lactose intolerance
– 40% of coeliac patients also have lactose intolerance (7)
–Type I diabetes
–Thyroid disease
–Anaemia
–Liver disease
–Osteopenia (weak bones)
How do you treat Coeliac disease?
The treatment of coeliac disease is simple – do not eat gluten. While this might sound easy, gluten is found in many foods and can be difficult to avoid.
Gluten is a plant protein found in wheat, barley, and rye.
The categorization of oats as containing gluten however is controversial. This partly relates to the contamination of oats with other gluten containing grains. The Australian Food Standards Code currently prohibits the use of a ‘gluten free’ claim on oat containing products. This contrasts with the situation in Europe, Canada, and the United States where oats that have been grown on ‘oat-only farms’ can be marketed as ‘gluten free’ (labelled ‘Pure Oats’).
Examples of wheat containing foods:
– Breads
– Pastas
– Cereals
– Biscuits and cakes
Examples of Barley containing foods include malts, and beer.
Rye is the least prevalent, mostly found in rye bread.
It is difficult to comply to a gluten-free diet as gluten can be present in many foods that we are unaware of. For example, gluten is used as a binder in many things we use every day. Gluten can be found in things like soya sauce, salad dressings, meat seasonings, potato chips, candy bars, luncheon meats, and soups. Interstingly and unexpectedly, gluten can also be found in toothpaste, lipsticks, vitamins/herbal supplements and even some prescription medications.
There are several important resources that can be helpful in adapting to a gluten free diet. The most valuable is an experienced dietitian who can help with education around reading food labels, learning to cook at home without gluten, eating-out strategies, recommended gluten substitutes and common pitfalls. The goal is to have a 100% gluten free diet. Another useful resource is the Coeliac Society of Australia. This organization provides lots of practical information, a regular newsletter and advocates for better awareness of coeliac disease.
Monitoring is important for people with coeliac disease. Yearly antibody testing is useful to assess for gluten exposure as this test should return to normal on a 100% gluten-free diet. Other blood tests monitoring for vitamin and mineral deficiencies is useful. A two yearly bone mineral density scan is also recommended.
Approximately 10% of the Australian population is gluten intolerant. This means that gluten causes significant and sometimes severe symptoms, however small bowel biopsies are negative for coeliac disease. The treatment of gluten intolerance is a diet with a reduced amount of gluten (to the level that symptoms no longer occur). A strict gluten-free diet is not necessary in gluten-intolerance.
- Kumar Pallav, Toufic Kabbani, Sohaib Tariq, Rohini Vanga, Ciaran P. Kelly, and Daniel A. Leffler Clinical utility of celiac disease associated HLA testing Dig Dis Sci. 2014 Sep; 59(9): 2199–2206.
- Singh P, et al. “Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis” Clinical Gastroenterology and Hepatology
- Ivarsson A, Persson LA, Nyström L, Ascher H, Cavell B, Danielsson L, Dannaeus A, Lindberg T, Lindquist B, Stenhammar L, Hernell O Epidemic of coeliac disease in Swedish children. Acta Paediatr. 2000 Feb; 89(2):165-71.
- F. MeloniS. Dessole N. Vargiu P.A. Tomasi S. Musumeci The prevalence of coeliac disease in infertility Human Reproduction, Volume 14, Issue 11, 1 November 1999, Pages 2759–2761,
- Alessio Fasano Clinical presentation of celiac disease in the pediatric population April 2005Volume 128, Issue 4, Supplement 1, Pages S68–S73
- Elias Zintzarasand Anastasios E. Germenis Performance of Antibodies against Tissue Transglutaminase for the Diagnosis of Celiac Disease: Meta-Analysis Clin Vaccine Immunol. 2006 Feb; 13(2): 187–192.
- CDHNF – NASPGHAN STATS (Dec 2010)

