Faecal Transplant
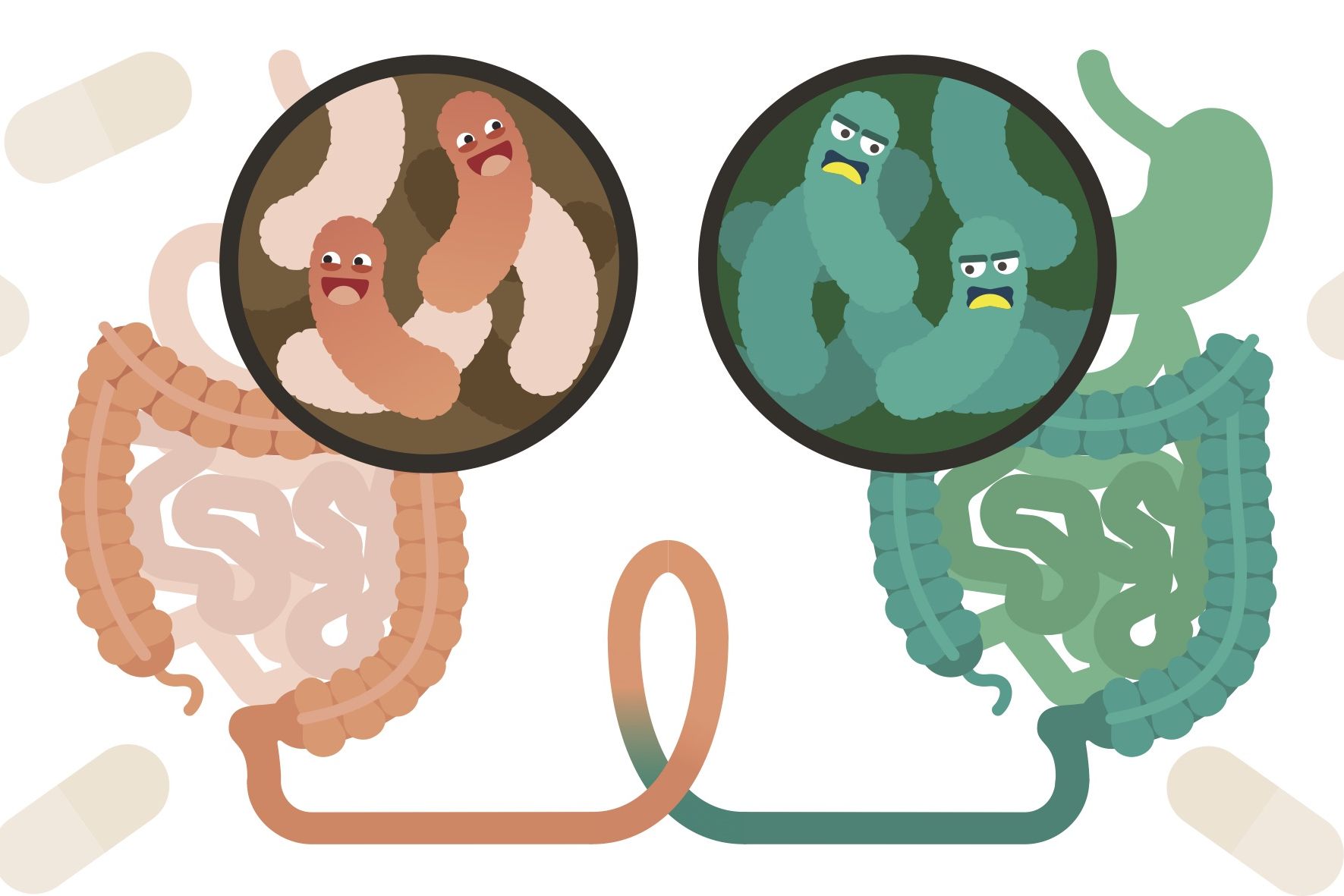
Faecal transplant, also call faecal microbiota transplant (FMT), is an exciting and emerging therapy in the field of Gastroenterology. Our gut bacteria also called the ‘ gut microbiome’, plays an important part in the healthy functioning of our immune system, digestion, metabolism and even mood.
What exactly is the gut microbiome?
When a change or imbalance in the gut microbiome occurs, called dysbiosis, a range of symptoms can occur. Gut symptoms such as bloating, pain and diarrhoea in particular are common. Faecal transplant is aim is to re-balance the gut microbiome.
How new is Faecal transplant?
Western medicine’s interest in faecal transplant however began in the 1950’s when a group of American surgeons used FMT to save the lives of 4 critically ill patients suffering from a specific bacterial infection of the bowel. Since that time there has been a growing amount of evidence for the use of faecal transplant.
Where can FMT be used in?
- Clostidium difficile: This is an opportunistic bacterial infection of the large bowel that often occurs when the normal gut microbiome is disturbed. This can happen when a patient is exposed to antibiotics and the “good” bacteria that protect the gut from infection are destroyed. Once C. difficile takes hold, it is often difficult to clear and can result in prolonged or recurrent bouts of infection. Current treatment consists of a course of antibiotics; however, this is typically only 30% effective in clearing C. difficile after a 14-day course of treatment. Often, patients find themselves on an endless cycle of antibiotics treatments, as the symptoms often recur as soon as the antibiotics are stopped. Restoration of the normal microbiome is needed and the most effective way to do this is FMT. There is significant evidence supporting faecal transplant in both acute and chronic C. difficile infections. (1)
- Ulcerative Colitis (UC): Affecting 1 in 400 Australians, UC is a chronic condition that causes inflammation in the large bowel. This can result in severe pain, diarrhoea and bleeding, and in severe cases can be life-threatening. Patients with UC are often required to take anti-inflammatory medications or injections that suppress the immune system for their entire life. There is now strong evidence that one of the main causes of UC is an imbalance of the bacteria living within the gut. Changing the gut bacteria to a profile more consistent with someone without any inflammation has the potential to change the underlying driver of UC. Four randomized control trials have been published that show a statistically significant clinical response with FMT is used in the treatment of UC treated. These figures compare favourably to the latest immunosuppressing medications that are both expensive, are required long term and may cause side effects. (2) Clinical trials evaluating the optimum preparation, mode of delivery and dosing schedule are ongoing.
- Irritable Bowel Syndrome (IBS): Irritable bowel syndrome is a common condition affecting at least 15% of the Australian population. It can be difficult to treat and is characterized by abdominal cramping, bloating and changes in bowel habit. An underlying bacterial disturbance has been identified as one of the components responsible for IBS symptoms. While results from recent clinical trials has been variable, three randomized controlled studies show a reduction in IBS symptoms. The most recent study published in late 2019 showed a significant decrease in symptoms in 89.1% of patients. (3) What was very impressive about this study was that a beneficial effect was seen in patients with all types of IBS: IBS-C (constipation), IBS-D (diarrhoea), and IBS-M (mixed).
- Obesity/Diabetes: Obesity and associated metabolic conditions such as diabetes is becoming a leading cause of health-related issues around the world. Recent data suggest that the gut microbiome plays an important role in energy and metabolism. (4) These also show that people with obesity and diabetes have a different microbiome profile than non-obese people. (5) Transplanting the microbiome from a lean person to someone suffering with obesity may prove to be a non-invasive and effective way to lose weight. There are also pre-clinical studies that suggest the potential for performance enhancement amongst marathon runners. (6)
Faecal Transplant has been used and is under active study in many neurologic and mental health diseases. This is due to the gut-brain axis and the role the gut microbiome plays in this pathway. Faecal transplant has been used in: Parkinson’s disease, autism, schizophrenia, anxiety/depression, Alzheimer’s disease, multiple sclerosis, fibromyalgia and chronic fatigue syndrome. Faecal transplant has also been used in the treatment of allergies.
How safe is Faecal Transplant?
Faecal Transplant is an exciting area of medicine and is likely to revolutionize the treatment of many diseases.
Gastro IQ has a faecal transplant program. The decision to proceed with this therapy is on a case by case basis, in consideration of the treatments already undertaken, the current evidence (always changing), and the goals of care. Detailed informed consent is involved in all cases. Participation in research trials may also be available.
References
- Fecal Microbiota Transplantation for the Treatment of Clostridium difficile Infection: A Systematic Review Cammarota, Giovanni MD; Ianiro, Gianluca MD; Gasbarrini, Antonio MD ournal of Clinical Gastroenterology: September 2014 – Volume 48 – Issue 8 – p 693–702
- Systematic review with meta-analysis: faecal microbiota transplantation for the induction of remission for active ulcerative colitis S. P. Costello | W. Soo | R. V. Bryant | V. Jairath| A. L. Hart|
- M. Andrews Alimentary Pharmacology and Therapeutics May 2017
- Efficacy of faecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study Magdy El-Salhy, Jan Gunnar Hatlebakk, Odd Helge Gilja, Anja Bråthen Kristoffersen, Trygve Hausken Gut Microbiota Dec 2019
- Drapkina OM, Korneeva ON. Gut microbiota and obesity: Pathogenetic relationships and ways to normalize the intestinal microflora. Ter Arkh. 2016;88(9):135–142.
- Ley R.E., Turnbaugh P.J., Klein S., Gordon J.I. Microbial ecology: human gut microbes associated with obesity. Nature. 2006;7122:1022–1023
- Meta-omics analysis of elite athletes identifies a performance-enhancing microbe that functions via lactate metabolism Jonathan Scheiman, Jacob M. Luber, Theodore A. Chavkin, Tara MacDonald, Angela Tung, et al Nature Medicine volume 25, pages1104–1109(2019)

